Many women experience intense period pain, heavy bleeding, or ongoing fatigue, yet they often dismiss these as “normal” parts of menstruation. These symptoms can quietly disrupt daily life, work, relationships, and overall well-being for years without a clear explanation. The good news? Greater awareness can lead to earlier support and practical ways to feel better. In this article, you’ll discover key insights into endometriosis and realistic steps that many women find helpful—plus one surprising lifestyle factor that research increasingly links to symptom relief.

What Is Endometriosis?
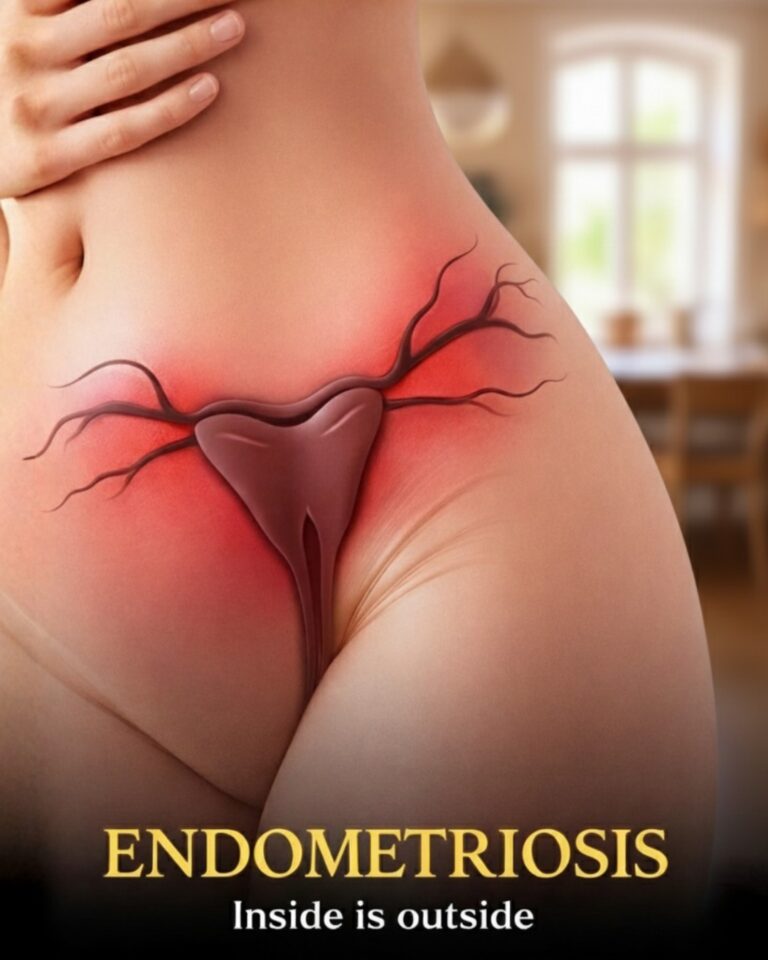
Endometriosis is a common condition where tissue similar to the lining of the uterus grows in other places, such as the ovaries, fallopian tubes, or pelvic lining.
During each menstrual cycle, this tissue responds to hormonal changes just like the uterine lining: it thickens, breaks down, and attempts to shed. However, unlike normal menstrual flow, it has no way to leave the body.
This trapped tissue can lead to inflammation, irritation, and the formation of scar tissue over time. While it affects an estimated 10% of women of reproductive age worldwide, many cases go unrecognized for years.
Common Symptoms Women Experience
Symptoms vary widely from person to person, which is one reason awareness matters.
Here are some of the most frequently reported signs:
- Severe menstrual cramps that worsen over time or don’t improve with usual pain relief
- Chronic pelvic pain that persists beyond menstruation
- Pain during or after intimacy
- Heavy periods or spotting between cycles
- Digestive discomfort, such as bloating, nausea, or bowel changes during periods
- Ongoing fatigue or low energy
Because these overlap with other common conditions, many women wait 7–10 years on average before receiving clarity, according to various health organizations.

But that’s not all…
Some women notice pain in the lower back, legs, or even during urination or bowel movements. Recognizing patterns early can make a real difference.
Possible Factors That Contribute to Endometriosis
Researchers continue to study why endometriosis develops. While the exact cause remains unclear, several factors appear to play a role:
- Retrograde menstruation — when menstrual blood flows backward into the pelvic cavity
- Genetic predisposition — having close family members with the condition increases likelihood
- Immune system differences that may affect how the body handles misplaced tissue
- Hormonal influences, particularly estrogen, which supports tissue growth
Importantly, endometriosis is not linked to personal lifestyle choices, and it’s not contagious.
How Healthcare Providers Identify Endometriosis
Getting answers often starts with an open conversation with a doctor.
Typical steps include:
- A detailed review of symptoms and medical history
- A pelvic exam to check for tenderness or unusual findings
- Imaging tests like ultrasound or MRI to visualize the pelvis
In some cases, minimally invasive surgery (laparoscopy) provides the most definitive view. Early discussions with a specialist can shorten the path to understanding what’s happening.

Endometriosis and Fertility: What the Research Shows
Endometriosis is associated with challenges in conceiving for some women.
Studies suggest that 30–50% of women with endometriosis may experience difficulty getting pregnant. Scar tissue can affect the fallopian tubes, and inflammation may interfere with ovulation or implantation.
Here’s the encouraging part: many women with endometriosis still achieve pregnancy naturally or with medical assistance, and go on to have healthy babies.
Practical Ways to Manage Daily Symptoms
While there’s no one-size-fits-all approach, several evidence-based strategies help many women feel more comfortable.
Pain and Discomfort Relief Options
- Over-the-counter anti-inflammatory medications (like ibuprofen) taken at the first sign of pain
- Applying gentle heat with a heating pad or warm bath
- Gentle movement such as walking, yoga, or swimming
Hormonal Management Approaches
Healthcare providers may discuss hormonal options that reduce or pause menstruation, which can lessen tissue activity for some women.
Surgical Considerations
In moderate to severe cases, surgery to remove visible endometrial-like tissue can provide significant relief, though symptoms may return over time.
Everyday Lifestyle Habits That May Help
Research points to several daily habits that appear supportive:
- Regular moderate exercise to improve circulation and reduce inflammation
- Prioritizing quality sleep and stress-reduction techniques like mindfulness or deep breathing
- Eating a balanced diet rich in fruits, vegetables, whole grains, and omega-3 sources
One area gaining attention is the potential role of diet. Some studies suggest that reducing red meat and processed foods while increasing fiber and anti-inflammatory foods (like berries, leafy greens, and fatty fish) may ease symptoms for certain women.
Could Diet Make a Difference?
Emerging research explores how nutrition influences inflammation and hormone balance.
Findings from observational studies indicate:
- Higher intake of fruits, vegetables, and omega-3 fatty acids is associated with lower symptom severity in some women
- Diets high in trans fats or red meat may correlate with increased risk
- Fiber-rich foods support healthy estrogen metabolism
While diet alone doesn’t change the condition, many women report feeling better with mindful eating patterns.
Here’s a simple starting point many find helpful:
- Add one extra serving of colorful vegetables to each meal
- Choose whole grains over refined options
- Include sources of healthy fats like avocado, nuts, or olive oil
- Stay hydrated throughout the day
- Track how different foods affect your symptoms for a few cycles
Small, sustainable changes often feel more manageable than major overhauls.
Living Well With Endometriosis
Managing a long-term condition takes patience and support.
Connecting with others through support groups or online communities can reduce feelings of isolation. Talking openly with partners, family, or trusted friends also helps.
Most importantly, working closely with a knowledgeable healthcare provider ensures an individualized plan that fits your life.
Frequently Asked Questions
How common is endometriosis?
It affects approximately 1 in 10 women of reproductive age globally, though exact numbers vary due to diagnostic challenges.
Can endometriosis go away on its own?
Symptoms sometimes improve after menopause when estrogen levels naturally decline, but tissue may remain.
When should I see a doctor about painful periods?
If pain regularly interferes with daily activities, work, or school, it’s worth discussing with a healthcare provider sooner rather than later.
Disclaimer: This article is for informational purposes only and is not medical advice. Always consult a qualified healthcare professional for personal health concerns, diagnosis, or management options.